30 | Tessa
“They pretty much all collectively agreed that it was probably best to go back to the mother-baby unit with my beautiful boy, Tommy... When I was there prenatally, I said to him in my tummy, ‘We’re not coming back here. I promise you, you won’t have to grow up and have your first couple of weeks here.’ And that’s what shattered me the most, was I felt like I was going back on a promise that I made.”
When Tessa was admitted to a mother-and-baby psychiatric unit during pregnancy, she made her unborn baby a promise that they’d never have to return. Unfortunately, the challenges of early postpartum and the pressures of perfection only compounded until she and her new born son were readmitted to her ‘little safe haven’ the MBU - not once, but twice.
This is one mother’s captivating story about finally accepting the need for additional support in its many forms, about letting go of shame and guilt, about coming to terms with a new diagnosis, and about the life-saving impacts that a quality care team can make.
Above all, this is Tessa’s story about looking back and seeing just how far she’s actually come.
“It's a hell of a story, but I think getting this story out there is a really important thing.”
“I would have been about four weeks along when I found out I was pregnant. The pregnancy happened a bit quicker than we thought it would. So I think it was a bit of a shock. And then I developed HG.”
“Trying to still continue to work, as well as the hormones really starting to ramp up, was just a massive shock to the system. There was just no warning. It was just bang. It mentally took a massive toll.”
“It felt like one thing after another. It felt like it was never going to get any better.”
“People, everyone, they're like, ‘Oh, how are you enjoying pregnancy?’ And you're like, ‘oh, it's great. It's fabulous.’ Inside you, it's like, ‘This is actually the worst, the worst experience I've ever had in my life.’ But you can't say that… I was still in that mindset of, ‘oh, no, I could never say that. I I can't say that. It's not proper to say those things.’”
“It just kept bottling up and bottling up. And I think that's probably how it all exploded on me.”
“I know the symptoms. I knew I was unwell. I just didn’t know how unwell I actually was.”
“Previously, before I was pregnant, I had an extensive mental health history. I had depression, I had anxiety. And being a nurse, I was feeling better and I was like, ‘I don't need to do this and I don't need to take this. And surely I don't have to do this follow up.’ And that really bit me where it hurt.”
“Like you're feeling really low, not wanting to interact with people. You're feeling quite ill, like feeling nauseated. When I think about it, the nausea and the HG, I actually think, well, I was more nauseated from feeling so unwell mentally. And it was just a massive explosion of my mental health and me.”
“So the dark thoughts, just everything just came creeping back.”
“I was at work one day and I was like, ‘I actually, I can't keep going on the way I am.’”
“I think, luckily, I have a little bit of insight. I know the symptoms. I knew I was unwell. I just didn't know how unwell I actually was.”
Tessa eventually presented to her GP for help. “So I started feeling a bit unwell. I think it was 17 weeks when I realised I really wasn't doing too well. I went to him. Obviously, he knew about my past history. We worked really well together with that.”
Her GP recommended that Tessa commence anti-depressants. “I was a bit stubborn and I said, ‘Oh, no, I'm not doing it. I'm not taking them again.’ Because you just have that pride of not taking tablets. And in that moment, you're like, ‘No, I'm not that unwell. I don't need to take that.’”
“Then he referred me to the perinatal mental health team. I had outpatient appointments with them via Telehealth. I think the lovely lady that I saw, I think we had maybe three sessions or four sessions before she goes, ‘I think it's time to do something. I just don't think you're getting any better.’”
Both Tessa’s GP and contact with mental health outpatient team mentioned the local mother-and-baby unit (MBU) as an option - living in rural Victoria, the MBU was approximately two and a half hours away from Tessa’s home, although that was not her primary concern.
“I was thinking, ‘oh my gosh, they're going to put me in a psych unit’. Unfortunately, I'd been in an acute adult unit before pregnancy, and it was the most terrifying experience of my life. So I was just like, ‘I'm not going. I can't go through that again. That was just horrible.’”
“They actually were really supportive of that.”
“And yeah, she goes, ‘Oh, look, why don't you and your partner come down? Just come and have a look. Bring your things and you can choose whether you want to stay with us… you're not locked up. You don't have to stay here if you don't want to. If you don't feel comfortable, you can go home.’”
“I went down there and I think I ended up staying maybe two and a half weeks.”
“I was gobsmacked... I think I did live in a bit of a denial for a little bit because I didn’t want to admit that.”
“I cannot fault them.”
Being pregnant in an MBU, surrounded by mothers and babies, was a unique experience for Tessa. “Before I went in, I think there was a moment where I had some very distressing thoughts of harming my little bubba. And being around babies, it did start to trigger me a little bit. And they were trying to minimise that for me, but they were trying to also gently expose me. Just a little bit of exposure therapy.”
“It gave you a bit of, I want to say, a look into your future of what was going to happen. But they had set up activities for you to do. They actually did some to suit the prenatal people as well as the postnatal. So that was really good. You could actually relate to what they were teaching you and what they were exposing you to. And it was just, yeah, it was really such a supportive environment.”
Tessa’s admission led to a new, and unexpected, diagnosis - but one that made sense to her in hindsight - and which kickstarted her recovery.
“I'd always had a very rocky relationship with medication and too much pride to take it - all that stuff! So they came to another conclusion. Maybe my diagnosis was a bit off. And so they did actually diagnose me with bipolar. So that was my new diagnosis.”
“I was gobsmacked. I was like, ‘No, I don't have what’s explained to us in nursing school or on the TV, all that thing. But the way it was explained to me was, so there's one pole and that pole. One is just the lows, and then the other pole is the highs. She goes, ‘you sit in the middle where you creep your way up, but just you don't quite get to that manic’. And I didn't know that.”
“I think I did live in a bit of a denial for a little bit because I don't want to admit that. I don't want to say that at doctor’s and have them look at me differently. And I think that's probably just the inner negative talk.”
”It was maybe a week or so before I went, ‘okay, I'm ready to accept this now and I'm ready to accept that these medications are going to help no matter what - air quotations - stigma, is attached to these medications.’”
“So they were just like, ‘let's try these different medications’. Being a nurse, you're like, ‘I don't want to take these medications because only crazy people take them’. But once I actually took the time, just think about it, and once I started taking the medications at the mother-baby unit, I started getting rest, I started sleeping better and they started to kick in. I was just like, I'm actually feeling better.”
“I could see the relationship between all the CBT and the medications all working. In my head, I was just like, ‘yes, I really need to give these medications a good go. This is going to be beneficial to get me through this.’”
“To actually work through that and go, ‘This is why it hasn't worked for so long!’ I'm proud of it now, I'm happy that I have this diagnosis and it all makes sense, and you can accept it from there.”
“When I went in, there was just no hope. It was bleak. It was very bleak.”
“When I went in, there was just no hope. It was bleak. It was very bleak, I have to be honest. But those two and a half weeks of just, I think, rest were yeah, massive.”
“The day when they said I could go home, I was like, ‘Oh, no, I’ve got to go home? I'm not going to look after myself!’ But I also had this renewed sense of, ‘All right, I can get through the rest of this pregnancy. That's all I've got to do. I've just got to get through.’”
“Unfortunately, I still had that negative aspect towards pregnancy, and that was never going to shift in such a small amount of time that I had left. But I was just like, ‘no, all I've got to do is I've got to get through until my maternity leave starts.’ And then we had things planned for those few weeks. I was an elective c-section because I needed the power to choose. So I had everything planned all up until that point. So I was always doing something. So I was always busy. And so they really set me up and gave me the tools to get me through to that point.”
“Obviously I had ongoing appointments with the perinatal team, through the mother-baby unit. I think I had them every week. I was hooked in with their psychiatrist. I don't know if she's still there or not. We had a beautiful psychiatrist. And yeah, so I think I saw we did telehealth appointments every week, just checking in. My GP was also my obstetrician. So he was also checking in every, I think I had GP appointments every week. I had midwife appointments. Yeah, I had check-ins with them.”
Throughout her admission and discharge during this admission as well as subsequent admissions in postpartum, Tessa is grateful for the support of her husband and family. “They were extremely supportive. I was glad I had my village. And that's my motto of always having your village so close. And the Mother Baby unit facilitated it. It was just amazing. Partners were encouraged, basically. They were just like, this is a part of your healing, basically. This is how we're going to get you to a point where you can go home is integrating you with your village, with your family, and with your support… They integrated everything. So when I went back into the community, it was all just there and all my supports were there.”
“So I am a nurse and I work where I gave birth. So I had a massive village of nurses and midwives all around me for that whole time, and then pretty much post-birth as well. So my village was quite big in the end. Once I started speaking up and once I started saying, ‘Look, things aren't right. And they're like, That's okay. That is okay to feel like that is a justified reason, and we'll be there for you.’”
“I remember sitting on the couch with him and just looking at him and just panicking and saying, ‘I can’t look after this baby.’”
“I had my little beautiful, beautiful baby, Tommy. He is now nine months old. Yeah, it was interesting. You don't really know how hard it is going to be until you have a baby. Working in that area, you see all these mums and they're doing so well and you're like, ‘it can't be that hard’. In your head, you don't say that out loud. But in my head, I'm just like, ‘Oh, I know what I'm doing.’ I definitely didn't know what I was doing.”
“They sent me home with this beautiful baby, and I'm just like, ‘what do I do now?’ And then just obviously, those couple of days after birth, the hormones all just stirred up again. And it all just went a little bit wrong again. So he was good. He was. He is a good baby. He just wasn't much of a sleeper. So I think that also took a toll because I'm one of those people that needed a good amount of sleep to function.”
“It's just a whole new world, and you'll get some people to go, ‘Oh, yeah, you're just tired because it's been a long couple of days’… I just couldn't cope with it. It was just a horrible little time.”
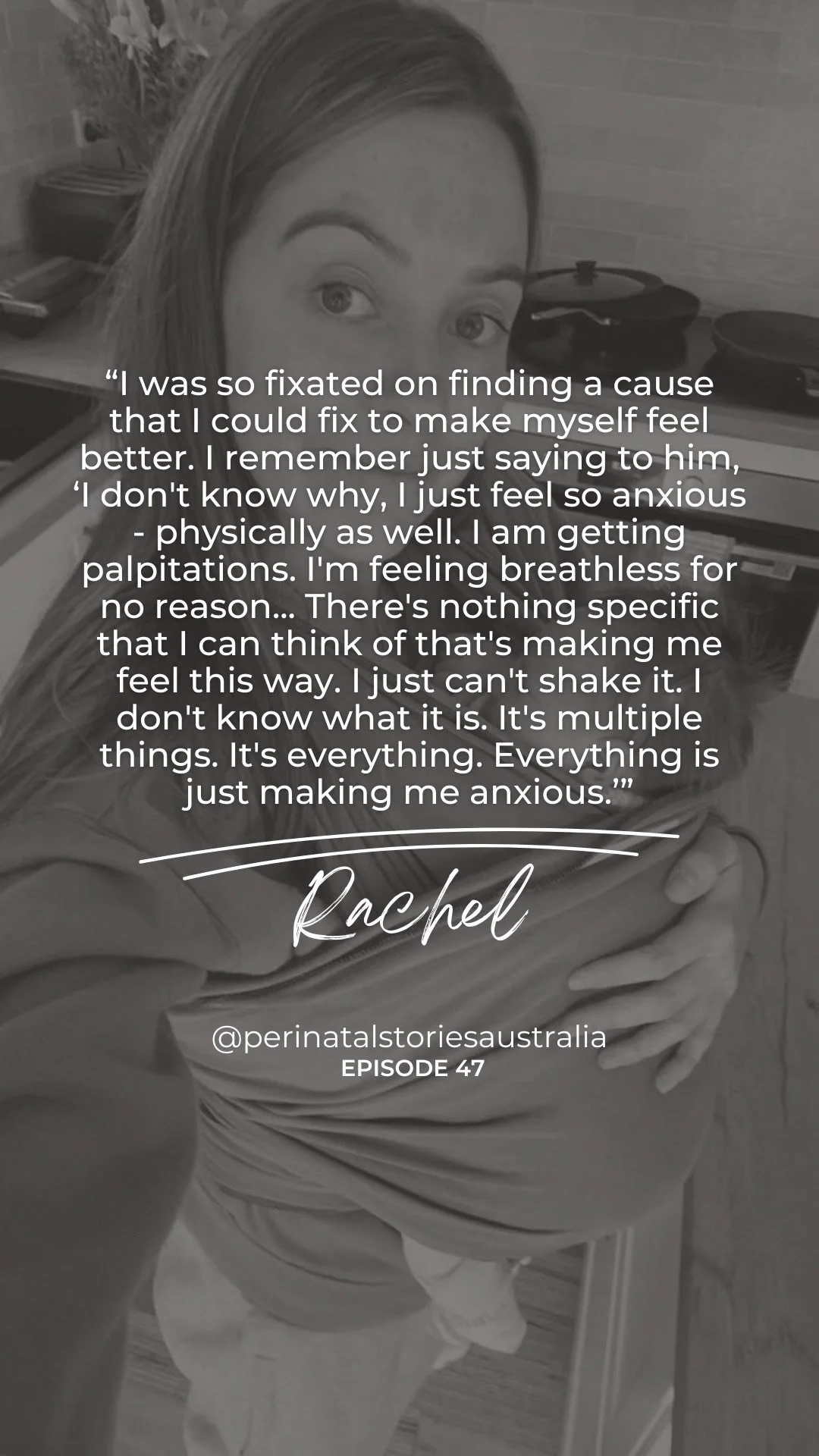
“I remember sitting on the couch with him and just looking at him and just panicking and saying, ‘I can't look after this baby’. It was just the moment that the anxiety just peaked. And it was, I think, the mother of all breakouts. My poor partner was there watching me unfold. And he was just like, ‘I didn't know how to help you at that point.’”
“Also, it was grief of losing myself. I felt like I was not myself. I'd lost. I was watching my friends. They were still doing what they wanted to do. They were still going to work. Work was my safe haven. It was where I wanted to be, and that's where I went to listen to other people's problems and not think about my own, which was probably not the healthiest coping mechanism I do get, but yeah, just like being home with this baby and then the thought of my partner going back to work and you're just sitting there holding this beautiful little baby, and you're going, ‘No, I can't do this. I can't do this by myself. How am I supposed to be doing this by myself?’”
“That was picked up by a couple of my friends who were going, ‘Are you okay?’ I'm like, ‘No, it's okay. I'm just really tired. Just the normal.’ But then I did start to notice the deeper it coming through again, just feeling sick, feeling lethargic. I actually think I had a cold. I think it lasted like really three weeks. And that's when I started to notice, ‘am I getting run down or is it the depression?’ It's really hard to differentiate because sometimes that's how it presents. So you keep pushing.”
“I think I cried for a good nearly 12 hours. When I was there prenatally, I said to him in my tummy, ‘We’re not coming back here. I promise you, you won’t have to grow up and have your first couple of weeks here.’ And that’s what shattered me the most, was I felt like I was going back on a promise that I made...”
Tessa was still being followed up by the perinatal outpatient team at the MBU.
“I think my partner had the phone number for the lovely lady that was looking after me, and he's going, ‘I’m not sure she's okay.’”
“I had appointments with them, the psychiatrist, my GP, and I think they pretty much all collectively agreed that it was probably best to go back to the mother-baby unit with my beautiful boy, Tommy, and have a bit of a stay and pretty much learn how to be a mum and cope with your mental illness.”
“I think I cried for a good nearly 12 hours. When I was there prenatally, I said to him in my tummy, ‘We're not coming back here. I promise you, you won't have to grow up and have your first couple of weeks here.’ And that's what shattered me the most, was I felt like I was going back on a promise that I made, and it actually still hurts me to this day. It shattered me.”
“I didn't think I was actually functioning at that point. I think it was just a bit of a shell of a person and just trying to push through for Tommy because I had to, but I just had nothing left. And obviously that was the only place that was going to be of help.”
“I was actually maybe six days, so I didn't last very long at home. I pushed for maybe a couple of days before I was just like, ‘no’. And then it all just hit me. Then I did start to accept it. I think a multitude of things were going wrong, and it was snowballing and there was just no stopping. So there was only one place we needed to go, our little safe haven.”
“I think I might have pushed myself to try and get myself out of the unit a little bit too quickly. I got that false sense of, Oh, yeah, no, I’ve got this. I’ve got this. I need to go home. I need to get my life into a routine. I’ve got to do this and I’ve got to do that. I think I put on a bit of a brave face and that didn’t get me very far.”
Although this was Tessa’s second admission to the mother-and-baby unit, it was a different experience to the last time when she was pregnant. This time, she had her newborn son with her.
“The first three days, they took bubs away and actually just allowed me to sleep the whole night because they just say, ‘oh, sleep is just the best thing’. And then you have those three days of just restorative sleep and you feel a million dollars after that. It's amazing.”
“They set you up and they'll help you overnight. They said to me, ‘Oh, we can do this for you. We can do this for you to ensure you get a good block of sleep’... We're going to work together to build me up to be able to cope with everything. Yeah, it was certainly different from that last admission.”
”Their groups were amazing… We'd have our babies. We'd all be in similar places or like some of us would be just at the start, someone would be at the middle or someone would be at the end. And you're sitting there and you can see, you'd be at the start and you can see these women and they've got their babies, and you can tell they're so close to being confident and just so close to being, I won't say happy, but ready to integrate back into the public. And you're just like, ‘so it is possible. It is possible to get there.’”
“And then you see a person that's just about to leave and you're like, ‘wow, is that what that looks like?’ I'm going to aim for that because that's where I want to be. I want to be at home with my mum and my family and all my support. Because being two and a half hours away is just ridiculous. I know the support of the nurses and all that stuff is really good, but nothing beats your village and the people that know you best.”
“[The other patients] were probably a massive factor of me getting better, just bonding with them over just the admission and where we were at in life. And even though we were all from different walks of life, our babies were different ages. It was just you all bonded, you all worked and put in the effort for these groups. And you talk about your babies, you talk about your life, and you talk about all your mental health adventures. And, yeah, you talk about all these things. And it's talk therapy. And it makes you feel better because it's just another human being that's exactly like you. And these things just happen. And you are only human. That's always my takeaway, you're only human. And it's unfortunate, but it's happened. And you just got to work through it.”
“I think we did mother crafting and cognitive behavioural therapy, a lot around the negative thoughts, learning how to change the way you're thinking, which is a massive thing for me because I'm a massive negative self-talker. That is my downfall. And so they explained it. You literally are trying to retrain your brain to think because you've been thinking like that for so long, you're going to have to do a lot of work. And they were right, actually. I'm not sure they'd love to hear this, but they were so actually right about it.”
“I think I might have pushed myself to try and get myself out of the unit a little bit too quickly. I got that false sense of, ‘Oh, yeah, no, I've got this. I've got this. I need to go home. I need to get my life into a routine. I've got to do this and I've got to do that.’ I think I put on a bit of a brave face and that didn't get me very far.”
“But we put on this bravado. We're like, ‘Oh, I can do this. I've been given the tools. I can do this. I've just got to practise it.’ And then when you get home, you don't practise it, and you don't do the things they tell you to do. And it all just crumbles again. These are the life lessons we have to learn, unfortunately, the hard way.”
“At that moment, you’re just stuck. And you’re just like, ‘is this what the rest of my life is going to be like?’ And you just see no other way out.”
“Coming home, I think I was rushed because I thought, ‘my poor partner, he only had six weeks off after bubs was born and he has not seen him at all.’ And so then all the negative thoughts, I felt guilty. I was like, ‘I'm keeping my baby from my partner, from my family. How could I be this selfish to take him away and only working on myself and only doing things for myself?’ And I think that also was the next thing that sent for my second admission.”
“I was just too focused on the themes of just guilt and just not sharing my baby… I was like, ‘I've got to go home. I've got to go do all these things. I've got to keep my house clean. When people come over, I've got to cook. I've got to do everything. And then I've got to work on myself. I got to do my mental health.’”
“You'd sit in your house, you'd look at things and you go, ‘I've got to do that’. And then you never do it. And you're just looking at it. It's just piling up and piling up. And you're like, ‘I should be able to do this.’ I don't understand why I can't go vacuum or go do the dishes or cook a meal or those kinds of things, these basic things.”
”Tommy had decided that he would only contact nap at that point, so he would not tolerate being put down for his sleeps. So he maybe contact napped for maybe 20 minutes or 30 minutes at a time every 2 hours. And so I was just like, ‘how do I get everything done?’”
“Then when you're feeding bubs or doing those quick contact naps, I'll be on my phone because I was like, well, there's no point shutting my eyes! It's just going to make me feel worse! And then, yeah, it goes on and on and ‘what if I drop him? What if I...?’ Yeah, all those kinds of negative thoughts.”
“And then you go on social media and you see those beautiful people with their beautiful babies and their beautiful houses. And you just like, ‘how? Why is that not happening for me? I should be able to do that. Why can't I do that?’ And in that head space, you can't ration with yourself to say, ‘that's actually just a picture.’ At that moment, you're just stuck. And you're just like, ‘is this what the rest of my life is going to be like?’ And you just see no other way out.”
“I couldn't do anything for myself. Everything was very, very dark at that point. And then to have people say, ‘oh, I think it's probably time to go back and try and get it all back to normal.’”
“I had those appointments over Telehealth. And in that month, that short month, they saw it…”
“Prior to that admission, I couldn’t hold him. I couldn’t look at him. I couldn’t feed him. I couldn’t do anything with him, which is horrible. And I would never wish that upon anyone.”
“I think at that point, I definitely accepted that it was another necessity.”
”Obviously, I have a beautiful supportive husband, but at that time, you're thinking, ‘he's going to leave me. He's going to hate me for taking bubs away again.’”
“It was also guilt of again taking my child away from my partner who then had to go back to work. So he wouldn't see us. He wouldn't see bubs. He wouldn't be able to create that bond with him. I'm in there trying to work on the bond with my baby because at that point, prior to that admission, I couldn't hold him. I couldn't look at him. I couldn't feed him. I couldn't do anything with him, which is horrible. And I would never wish that upon anyone.”
“At that admission, I realised I do need to start working and taking time for myself because you cannot look after bubs if you're not looking after yourself and you're not doing that self-care, it's just not a viable thing. And you can't live like that.”
A big component of Tessa’s second postpartum MBU admission was working on the negative thoughts that spiralled during the short month from when she was discharged last time.
“I always had thoughts of, ‘I'm not good enough to be his mother. Why would I think I could do this?’ Those things like, ‘I need to be doing this. I need to be perfect, basically. Everything must be perfect.’ So yeah, and actually learning to accept that it's okay. They said, ‘good enough parenting’. I think It's drilled into me now.”
“I was running on maybe giving 100% of myself because that's what was expected of me, in air quotation marks. That's what's expected of us. And that's what we have to do. And that's just normal. But it's not. And it's not reality. And I think the more we tell people, ‘no, it's okay. That's just not a viable thing. And you can't keep pushing yourself to do that.’”
“This time I felt this was actually going to work. Obviously, things were still a little bit rougher on the edges, but I had actually put my mind to it. I said, ‘no, this is the last time, we're not doing this again. We are going home, we're staying home, and we are having good family times.’ So that was my goal.”
“It was just also amazing to live and just look back on the journey that I had been on to get myself to this point. And you look down at this little bubba and go, ‘we're going home now and it's going to be all okay’. And taking in all those groups, all the lessons of being good enough parenting… having to put that into play when you get home is obviously it's a hard thing to do. But I think once if you've got that determination, that drive, you're feeling better. You've had sleep. You're on the right medications. You're talking to someone frequently. You're going to start feeling better. And it's just a whole new world.”
“It was an amazing difference between that first admission and the second one and going home because I had done the work - like the nice people had told me to!”
Prior to this discharge, Tessa participated in some trial nights, meaning she had leave overnight to practice returning home. “My parents were only about an hour away from the mother-baby unit, so they let me go there instead of going all the way home and then going back. So I had some overnight leave and just to try and reintegrate myself back into what a normal household would be. And that was, they were scary. I think I cried a lot. That's just normal. I think Baby and I cried together a little bit. But yeah, no, it was, it's a scary thought at the start.”
“I think that first admission I was thinking to the end and going, ‘that's where I need to be’. But if you start working on one day at a time, you can go one hour at a time if you really need to, that's where I started. You got an hour, then the next hour. Yeah, by that time, the day was over and everyone was still alive at the end of the day. So it was always a good day.”
“I actually think it’s one of the proudest moments of my life: looking back and going, I did make it through all that, even when I thought I didn’t. And when I said I couldn’t do it, I’ve done it, and I will continue to keep doing it.”
Since ‘doing the work’ as Tessa calls it, she has been discharged as an outpatient from the perinatal mental health team.
“You don't have to be perfect. You don't have to be... Yeah, And you're just working with that internal dialogue and obviously working with your support team, just making sure you follow up all your appointments, you take your medications, you have you-time.”
“I am now seeing a private psychiatrist and a private psychologist. So they are just as lovely, of course. They specialise in postnatal recovery. So basically, as bub grows, everything changes. And so we work through the milestones… just working through those little things like milestones and enjoying them instead of just saying, ‘oh, that's just another thing to tick off.’ He's doing this and not focussing too much on ‘he has to do this by this time and he has to do this’. And I think we also put too much pressure on ourselves and our babies to do things on time when people say that they have to do it. And that's also another hard thing to learn when you like things perfectly. So it's definitely been a big thing with me.”
“And I've just gone back to work and not feeling guilty about going back to work and not feeling guilty about putting him in day care and things like that because I didn't like people taking him from me to do things their way because it was all done. It was all done nicely and we figured out a pattern. We got really comfortable. And now this new thing where I went back to work and it's just changed everything again. So you've got to learn to adapt. And it's a massive thing. But he absolutely loves day care. So that makes it so much better.”
“I have changed dramatically. Obviously, being a nurse, you're still caring. You want to do the best for your patients. But you also realise it's just a job at the end of the day. You obviously love what you do, but you go home and you see a little bubba and you go, this is what I'm working for. This is the little person that I want to care for and look after.”
“And I was really career-driven before then. I wanted to work my way up and I wanted to be this person. And I did a postgraduate before Tommy was born. But I have no interest in doing that anymore.”
“Yeah, this is the first week back and I'm just like, ‘this is definitely not the Tessa I remember at work’. I would take so much work home with me and then now you just leave it at the door.”
”[The negative thinking is] also still a work in progress. I think that's going to be for a lot of my life. You still look at that pile of washing and you go, ‘I should do that’. But then you just like, ‘actually, it doesn't matter. Who cares? It'll get done eventually. Someone will do it.’ If you can look at something and think, I'll do that later, or it doesn't matter, you've grown.”
“And it's amazing to come on here and talk to someone - you just realise how much you've actually changed and how far you've actually come. And it's just... I actually think it's one of the proudest moments of my life is looking back and going, I did make it through all that, even when I thought I didn't. And when I said I couldn't do it, I've done it, and I will continue to keep doing it. And you're just so proud.”
“Thank you so much for letting me come on in and talk about it. It was just, yeah, you always want to, you want to put yourself out there, you want to support others. And you just don't know how to. You don't know where to start. But this is amazing.”
“I want people to know that there is light at the end of the tunnel. It does get better.”
Listen to the full episode:
Episode Sponsor
This episode is proudly brought to you by Tommee Tippee Australia. Tommee Tippee knows that for every newborn baby, there's a newborn parent too.
Tommee Tippee was founded over half a century ago, born from a mission to make life easier for parents. For decades they've been designing products that enhance a parent’s intuition, and engineering solutions to make caring for babies easier, simpler, and more instinctive. You’ve got this, we've got you.
Visit their website at tommeetippee.com.au to shop a range of equipment for the naturally equipped.
Sign up to become a VIP (a very important parent!) and get 15% off your first order.